Yes, it is important to inform the surgery center about any additional insurance plans you have for several reasons:
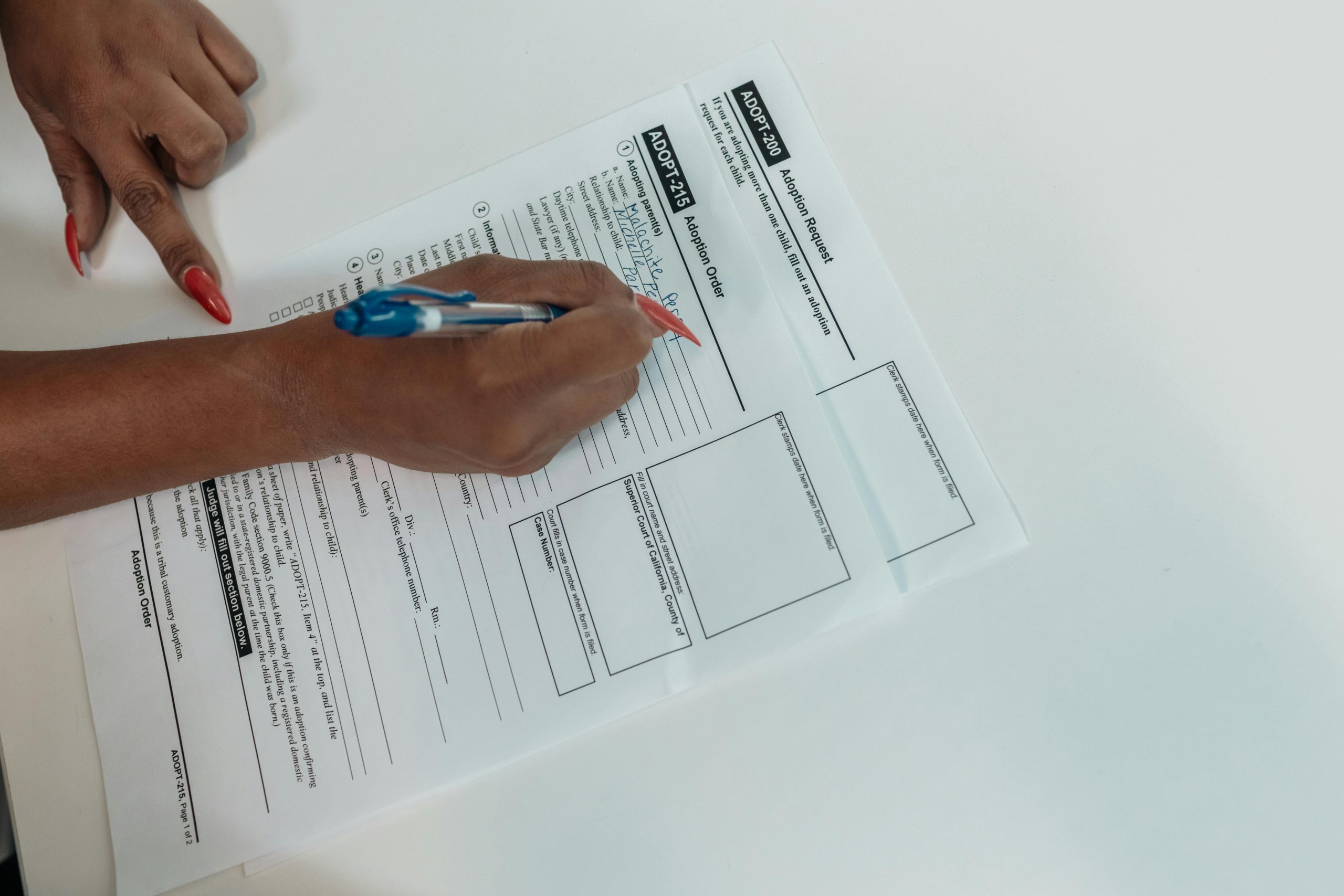
Coordination of Benefits: If you have more than one insurance plan, it’s crucial to determine which plan is the primary insurer and which is secondary. This process, known as coordination of benefits, helps ensure claims are processed correctly and that you make the most of your insurance coverage. Not disclosing all your insurance information might result in claims being denied or delayed.
Accurate Billing: By informing the surgery center of all your insurance plans, they can bill the correct insurer(s), reducing your out-of-pocket costs. Accurate billing prevents you from being charged unnecessarily for services that are covered by your insurance.
Minimizing Personal Expenses: Additional insurance plans can cover portions of costs that your primary insurance does not, such as deductibles, co-pays, or specialized treatments. Informing the surgery center ensures they can help you utilize all available resources to minimize your personal financial responsibility.
Compliance and Transparency: Medical and billing professionals rely on accurate information to comply with legal and contractual obligations with insurance providers. Transparency in your insurance coverage supports compliance with these regulations, avoiding potential legal or financial complications for you and the healthcare provider.
Efficient Processing: Providing complete insurance information upfront prevents administrative errors and avoids the need for later corrections, which can lead to billing errors and complications in claim processing.
By proactively disclosing all insurance information, you help facilitate a smoother and more efficient billing process and ensure you receive the full benefits you are entitled to.